Preventive Services Covered at 100%
Preventive care services are covered in full when you visit in-network providers.
However, you may be billed depending on the outcome of the service and the type of plan you have. In order to track each preventive visit and test, the provider sends a claim to the insurer, billing them for the service. Your health plan pays the total cost for your visit.
The ACA requires all plans to cover certain services for free, which should be listed in your schedule of benefits. Here are the key reasons why preventive care and billing are misunderstood.
Billing Code Issues
A good example of where confusion in billing often arises would be receiving a mammogram, which is a preventive service covered by all health plans.
However, the billing code could indicate the mammogram was a diagnostic service, therefore resulting in a bill. Preventive care is not to be billed, while diagnostic care can be. What distinguishes the two is that preventive care is intended for those who appear to be healthy, as a precaution. Diagnostic care is defined as care given to patients to determine the root of their symptoms.
One service can be in either category, though it is entirely dependent on the health status of the patient.
A woman who is in seemingly good health receiving a mammogram should be billed for a preventive service. A woman who received the service after noticing a lump in her breast should be billed for diagnostic care.
Clarifying this to a patient is very important, as they may see a service on the list of free preventive care benefits and assume it will not be charged if they are experiencing symptoms of an illness or condition. As a patient and health insurance policyholder, it is necessary to ask your doctors whether a service will be billed and what category it falls under.
When a Service is No Longer Preventive
Another example would be when a patient reaches the appropriate age where a colonoscopy is suggested as a preventative service.
If the patient had no symptoms and went to the physician as recommended by their health plan, and the test results show nothing irregular, it is a free service. The patient’s insurer would be billed, and all is well.
Conversely, suppose the test results came back irregular and a polyp was discovered, and the doctor decides to remove the polyp for further screenings. Having received an additional procedure and follow-up testing, this goes beyond preventative care. The service is then considered diagnostic, and therefore the patient should expect an additional bill.
Out-of-Network vs. In-Network
Out of network providers charge more for all services than your plan’s network.
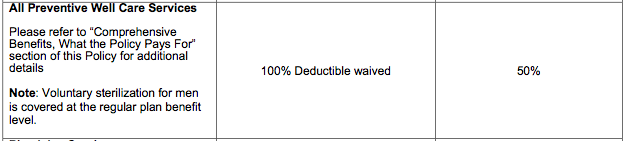
As you can see from a basic outline of benefits with in-network and out-of-network services side-by-side, out-of-network preventive services are not covered in full. It is crucial review your plan benefits and coverage before a visit.
Below is a sample from a health plan brochure:
Make sure you understand your plan and your schedule of benefits before receiving care, and before disputing with your providers or insurer.
It is also the job of the federal government and the health care system to be more clear on what is covered and what will not be. No one can assume a patient knows exactly what to expect. As a patient, you can inform yourself with the knowledge given by your plan so to avoid confusion regarding preventive care.

Leave a Comment